What is a Cataract?
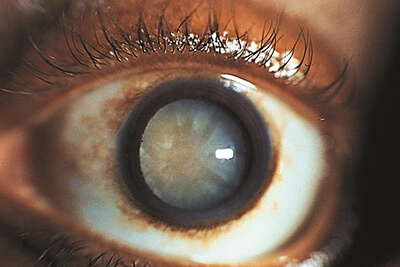
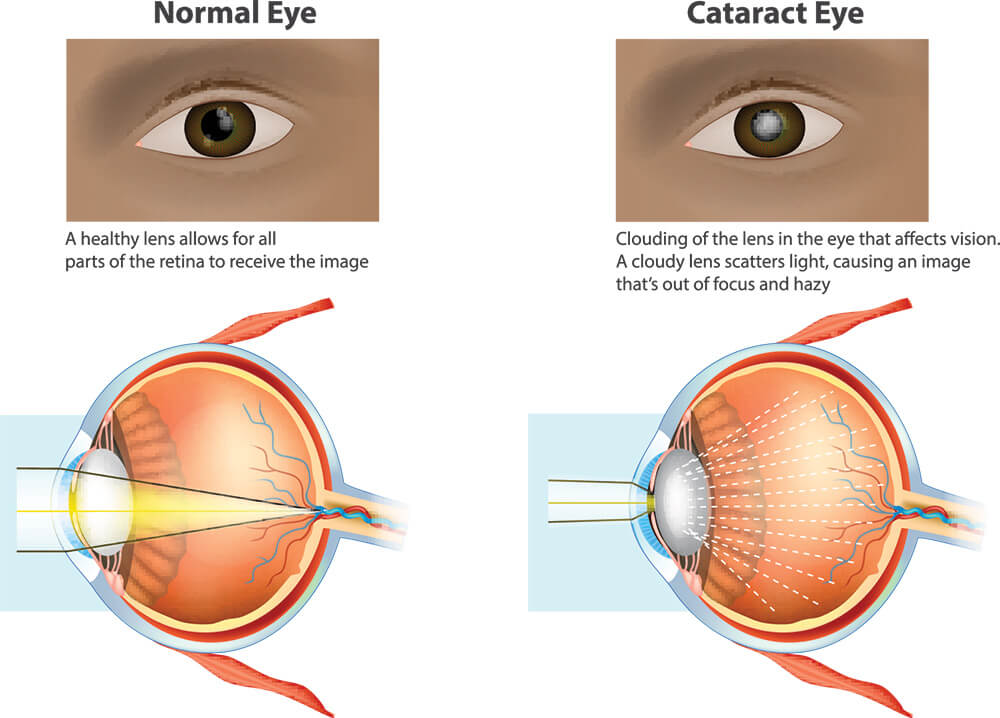
A cataract is hardening and clouding of the natural crystalline lens within your eyeball. It is a normal process of aging, but it can also occur in the setting of trauma or chronic steroid use amongst others. This process usually begins in your 40’s but patients often do not require surgery until after age 60. We also can see cataracts sooner in glaucoma patients secondary to chronic use of glaucoma drops or from previous glaucoma/eye surgery. The lens in the eye focuses light onto the retina and allows us to see. When this lens gets cloudy it results in a degradation of vision.
When someone develops a visually significant cataract they may experience:
- Clouded, blurred, or dim vision
- Increased difficulty with night vision
- Glare and halos around lights
- Sensitivity to light
- Need for increased light to read and perform other activities
- Changes in in contact lens or eye glasses prescriptions
- Colors fading, often appearing washed out or yellow
How is cataract surgery performed?
Removal of the cataract is an outpatient surgical procedure. It is done under light IV sedation and local/topical anesthesia. This allows for a lower risk procedure and easier recovery. Following the surgery you will have a clear shield placed over your eye and you will begin eye drops that day. You will see your doctor that afternoon or the following day for your first post operative visit.
Traditional cataract surgery:
Traditional (non laser) cataract surgery uses small incisions and is almost always sutureless. A tiny incision is made in the clear part of your eye called the cornea. A circular opening is made in the lens bag (capsule) which holds the cataract. An ultrasound probe (phaco) is placed through the incision into the eye and used to break up the cataract into several small pieces which are aspirated out of the eye. Additional cataract material is further removed from the eye using an irrigation-aspiration handpiece. Once all the lens material is cleaned out, an intraocular lens implant (IOL) is placed into the bag. The artificial lens implant is placed in the natural anatomic position where it will remain. If the capsular bag is unstable (which can be seen more commonly in some glaucoma patients), your doctor may choose to implant the IOL in a different position to ensure a stable lens.

